One technique, known as photothermal therapy (PTT), converts laser light into heat that can target and kill tumor cells. Another technique, photodynamic therapy (PDT), uses laser light to generate reactive oxygen species (ROS), such as hydroxyl radicals, singlet oxygen, superoxide radicals, and hydrogen peroxide, which can wreak devastation on tumor cells.
In Applied Physics Reviews, by AIP Publishing, a multinational team of researchers reviews the current status of the field of nanoparticle-enhanced PDT and PTT and focuses on combining the two techniques to achieve the highest level of treatment efficiency.
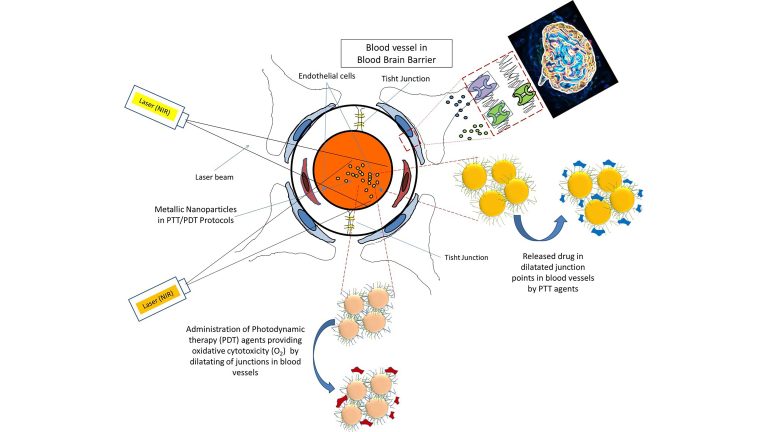
Combined PDT/PTT approaches for the treatment of brain tumors. Dual function nanoparticles are used for combined PDT/PTT approaches. In PDT, the PS to produce ROS can be attached to nanoparticles and delivered to the tumor. The combination of nanoparticles and irradiated laser beam increases the permeability of the microvessels to transfer nondiffusible drugs across the vessel wall.
By combining PTT or PDT with nanomaterials, investigators have been able to apply these types of phototherapies while also delivering drugs to sites in the body that are otherwise inaccessible. It is also possible to combine PTT and PDT into a single treatment, creating an even more powerful treatment method.
The surface of the nanoparticle can be modified to attach a photosensitive molecule to the surface. This allows the absorption of light at a particular wavelength. In the PTT method, this light is converted to heat. In PDT, the light creates ROS. For PDT to be successful, sufficient ambient oxygen must be present to produce enough ROS to kill tumor cells.
“In cancer therapies using this strategy, the penetration depth of laser light into the tissues is critical in determining the therapeutic efficiency,” said author Masoud Mozafari, from the Iran University of Medical Sciences.
Factors that control the penetration depth include the shape of the beam, wavelength of the light, intensity of the laser, and the radius of the beam.
A powerful approach is to combine PDT with traditional medical treatments, such as chemotherapy, to create photodynamic antibacterial chemotherapy.
The nanoparticles can be used to deliver chemotherapeutic agents or antibiotics to the tumor site. When light is applied, generating ROS molecules in the tumor and killing both tumor cells and bacteria, the antibiotics can be released to prevent infection in the treated area.
Other modifications to the nanoparticle surface could allow it to cross the blood-brain barrier so that brain tumors can be treated.
One set of studies reviewed in this work involved gold nanorods that had a glycoprotein from the rabies virus attached to their surface. Since this virus naturally infects the brain, the gold nanorods were able to penetrate the blood-brain barrier and target the brain tumor. Applying light from a laser then allowed the nanorods to generate localized heat, killing the tumor cells.
These techniques can also be used to treat other medical issues, such as atherosclerosis, scar removal, abscesses, nonhealing ulcers, or dental infections.
Read the original article on AIP Publishing.