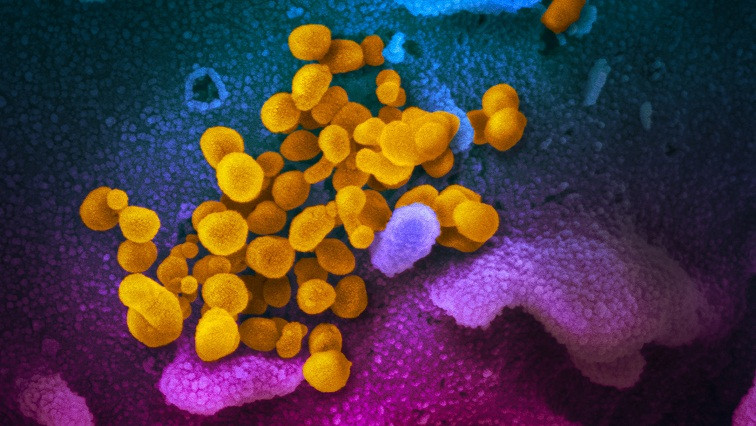
As more Covid-19 cases appear in the United States and around the world, the need for fast, easy-to-use diagnostic tests is becoming ever more pressing. A startup company spun out from MIT is now working on a paper-based test that can deliver results in under half an hour, based on technology developed at MIT’s Institute for Medical Engineering and Science (IMES).
Cambridge-based E25Bio, which developed the test, is now preparing to submit it to the FDA for “emergency use authorization,” which would grant temporary approval for using the device on patient samples during public health emergencies.
Elsewhere around MIT, several other research groups are working on projects that may help further scientists’ understanding of how coronaviruses are transmitted and how infection may be prevented. Their work touches on fields ranging from diagnostics and vaccine development to more traditional disease prevention measures such as social distancing and handwashing.
The technology behind the new E25Bio diagnostic was developed by Lee Gehrke, the Hermann L.F. von Helmholtz Professor at IMES, and other members of his lab, including Irene Bosch, a former IMES research scientist who is now the CTO of E25Bio.
For the past several years, Gehrke, Bosch, and others in the lab have been working on diagnostic devices that work similar to a pregnancy test but can identify viral proteins from patient samples. The researchers have used this technology, known as lateral flow technology, to create tests for Ebola, dengue fever, and Zika virus, among other infectious diseases.
The tests consist of strips of paper that are coated with antibodies that bind to a specific viral protein. A second antibody is attached to gold nanoparticles, and the patient’s sample is added to a solution of those particles. The test strip is then dipped in this solution. If the viral protein is present, it attaches to the antibodies on the paper strip as well as the nanoparticle-bound antibodies, and a colored spot appears on the strip within 20 minutes.
Currently, there are two primary types of Covid-19 diagnostics available. One such test screens patient blood samples for antibodies against the virus. However, antibodies are often not detectable until a few days after symptoms begin. Another type of test looks for viral DNA in a sputum sample. These tests can detect the virus earlier in the infection, but they require polymerase chain reaction (PCR), a technology that amplifies the amount of DNA to detectable levels and takes several hours to perform.
“Our hope is that, similar to other tests that we’ve developed, this will be usable on the day that symptoms develop,” Gehrke says. “We don’t have to wait for antibodies to the virus to come up.”
If the U.S. Food and Drug Administration grants the emergency authorization, E25Bio could start testing the diagnostic with patient samples, which they haven’t been able to do yet. “If those are successful, then the next step would be to talk about using it for actual clinical diagnosis,” Gehrke says.
Another advantage of this approach is that the paper tests can be easily and inexpensively manufactured in large quantities, he adds.
RNA vaccines
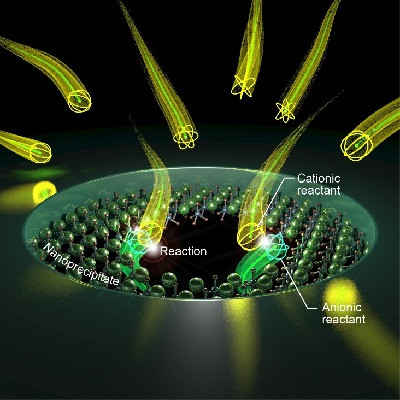
On Feb. 24, only about a month after the first U.S. case of coronavirus was reported, the Cambridge-based biotech company Moderna announced it had an experimental vaccine ready to test. That speedy turnaround is due to the unique advantages of RNA vaccines, says Daniel Anderson, an MIT professor of chemical engineering, who also works on such vaccines, though not specifically for coronavirus.
“A key advantage of messenger RNA is the speed with which you can identify a new sequence and use it to come up with a new vaccine,” Anderson says.
Traditional vaccines consist of an inactivated form of a viral protein that induces an immune response. However, these vaccines usually take a long time to manufacture, and for some diseases, they are too risky. Vaccines that consist of messenger RNA are an appealing alternative because they induce host cells to produce many copies of the proteins they encode, provoking a stronger immune response than proteins delivered on their own.
RNA vaccines can also be quickly reprogrammed to target different viral proteins, as long as the sequence encoding the protein is known. The main obstacle to developing such vaccines so far has been finding effective and safe ways to deliver them. Anderson’s lab has been working on such strategies for several years, and in a recent study he showed that packing such vaccines into a special type of lipid nanoparticles can enhance the immune response that they produce.
“Messenger RNA can encode the viral antigens, but in order to work, we need to find a way to deliver these antigens to the correct part of the body so that they get expressed and generate an immune response. We also need to make sure that the vaccine causes appropriate immune stimulation to get a strong response,” Anderson says.
Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases (NIAID), has estimated that it will take at least 12 to 18 months to fully test any potential Covid-19 vaccine for safety and effectiveness.
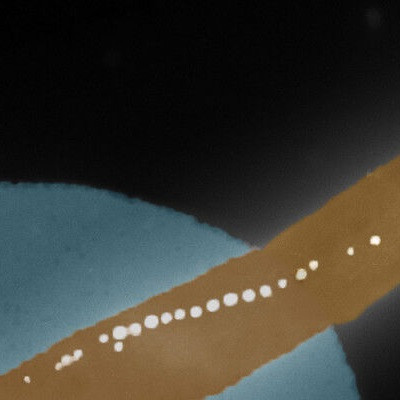
Keep your distance
Over the last decade, Lydia Bourouiba, an associate professor directing the Fluid Dynamics of Disease Transmission Laboratory at MIT, has focused on characterizing and modeling infectious disease dynamics and transmission at various scales. Through experiments in the lab and clinical environment, she has reported that when a person coughs or sneezes, they do not emit a spray of individual droplets that quickly fall to the ground and evaporate, as scientists had once thought. Instead, they produce a complex cloud of hot and moist air that traps droplets of all sizes together, propelling them much further through the air than any individual droplet would travel on its own.
On average, her experiments have revealed that a cough can transmit droplets up to 13 to 16 feet, while a sneeze can eject them up to 26 feet away. Surrounding air conditions can act to further disperse the residual droplets in upper levels of rooms.
Bourouiba notes that the presence of the high-speed gas cloud is independent of the type of organism or pathogen that the cloud may contain. The droplets within it depend on pathogenesis coupled with a patient’s physiology — a combination which her laboratory has focused on deciphering in the context of influenza. She is now expanding her studies and modeling to translate the work to Covid-19, and says now is a critical time to invest in research.
“This virus is going to stay with us for a while — and certainly data suggest that it is not going to suddenly disappear when the weather changes,” she says. “There’s a fine and important balance between safety, precautions and action that is important to strike to enable and dramatically accelerate research to be done now so we can be better prepared and informed for actions in the weeks and months to come when the worst of the pandemic will unfold.”
She is also working with others to evaluate ways to limit a cloud’s dispersal and slow Covid-19 transmission to health care workers and others in shared spaces. “A surgical mask is not protective against inhalation of a pathogen from the cloud,” she says. “For an infected patient wearing it, it can contain some of the forward ejecta from coughs or sneezes, but these are very violent ejections and masks are completely open on all sides, and fluid flows through the path of least resistance.”
Based on the data, she recommends that health care workers consider wearing a respirator, whenever possible. And, for the general public, Bourouiba emphasizes that the risk of contracting COVID-19 remains relatively low locally, and that risk should be thought of in the context of the community.
Wash those hands
Another good way to protect yourself against all of those tiny infectious droplets is to wash your hands. (Again, and again, and again.) Ruben Juanes, an MIT professor of civil and environmental engineering, and of earth, atmospheric and planetary sciences, published a study in December showing the importance of improving rates of handwashing at key airports in order to curtail the spread of an epidemic. Now, he says, following the Covid-19 outbreak, governments around the world have imposed unprecedented restrictions on mobility, including the closure of airports and suspension of flight routes.
At the same time, the World Health Organization, U.S. Centers for Disease Control, and many other health agencies all recommend hand-hygiene as the number one precaution measure against disease spread. “Following our recent paper on the impact of hand-hygiene on global disease spreading,” Juanes says, “we are now investigating the combined effect of restrictions on human mobility and enhanced engagement with hand-hygiene on the global spread of COVID-19 through the world air-transportation network.”
Juanes says he and Christos Nicolaides PhD ’14, a professor at the University of Cyprus who was the lead author of the previous study, are working “with fine-grained, worldwide air-traffic data that accounts for all flights for the period between Jan. 15, 2020 until today (accounting for closures/cancellations) and the corresponding period of 2019 (base level) to elucidate the role of travel restrictions on the global spread of Covid-19 through detailed epidemiological modeling.”
“Furthermore,” he adds, “we simulate different hand-hygiene strategies at airports on top of travel restrictions with the goal of proposing an optimal strategy that combines travel restrictions and enhanced hand hygiene, to mitigate the advance of Covid-19 both in the short term (weeks) and the long term (the next flu season).”
Juanes says they will make the results immediately available via medarXiv, while the work follows peer-review in a journal. This would also allow the information to reach other academic and government institutions in a more timely way, he says.
Read the original article on MIT News.