Icosavax’s translation of synthetic virus-like particles (VLPs) into key elements in a vaccine for respiratory syncytial virus (RSV) was sufficiently novel – and the company well-funded – that Nature Biotechnology recently listed it among the “best science that was commercialized from academia in 2019.” As a platform, it holds promise as a solution to developing vaccines against a number of intractable viruses such as HIV, cancer and malaria.
“VLPs have special immunological properties and are processed differently by the immune system so they have longer duration,” Adam Simpson, CEO of Icosavax, told BioSpace. Because they contain no genetic material from the virus, they are safer than either live-attenuated or inactivated vaccines.
“If you could have an inert, safe particle that has a repetitive structure (so it looks like a virus), your body has a warning system. We know VLPs can be some of the most effective vaccines that are commercialized because of this repetitive nature,” Simpson said.
The value of naturally occurring VLPs is evident in vaccines targeting human papillomavirus (Gardasil® and Cervarix®) and Hepatitis B (Engerix-B® and Recombivax HB®).
VLPs haven’t yet been used to target complex heterologous antigens like those involved in RSV. The challenge has been to find a way for VLPs to address a wide range of targets for which there are no naturally-occurring VLPs. Specifically, Simpson said, “The problem has been to engineer a particle to present antigens of interest that are manufacturable and scalable.”
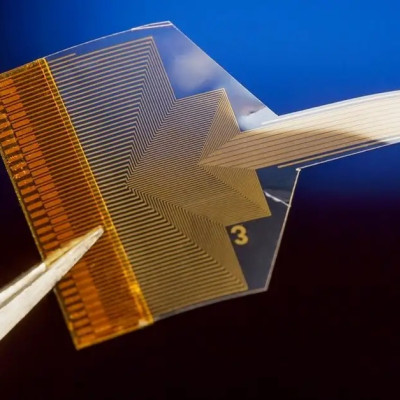
Technology developed at the University of Washington’s Institute for Protein Design (IPD) and licensed by Icosavax, has solved the problem. Basically, the VPL vaccine is designed in two parts that self-assemble.
As Neil King, Ph.D., chair of the company’s scientific advisory board, and assistant professor at the IPD, elaborated, “The nanoparticles are built from two different protein building blocks, like the black and white pentagrams and hexagrams on a soccer ball.”
Armstrong, continuing the soccer ball analogy, added, “The soccer ball is the core of the vaccine, and the antigens stick out of the black parts of the ball.”
“We use Rosetta software to take these proteins and arrange them in 3D space to form nanoparticles in the structure we want,” King said. “We program the blocks to stick to each other to form a physical structure by mutating the amino acid sequences. With 20 letters, those sequences can be infinitely more complex than those of DNA.”
Each of the two proteins is built separately. “They can’t assemble until they are mixed together in a test tube,” King said. This separates the folding of individual protein subunits from the assembly of the final macromolecular structure. “If they were allowed to assemble as the antigens were starting to unfold, well…that’s where things break down. By splitting development and assembly, the antigen can fold its complicated structures and we can control when the particles assemble.”
Folding is important, Simpson elaborated, because, “The antigen for certain diseases are complex in their own right and must be folded properly to display the right parts to be regulated by the immune system.”
The magic of the technology is its engineering. Using the soccer ball analogy that he and King find so apt, Icosavax has to engineer both the black and white parts of the structure, cause the recombinant antigen connect to the black part, and then combine the black and white portions in a way that forces the antigens to stick out.
Among the many intractable viruses for which nanoparticle VLP-based vaccines could be applied, Icosovax chose respiratory syncytial virus. The reason is the urgent need.
“There is no vaccine for RSV, but it causes approximately 160,000 deaths per year,” Simpson said. RSV is the viral trigger to pneumonia. Like the seasonal flu, those with weakened immune systems are most at risk.
“In the U.S., the problem is more pronounced in adults aged 65 and older. In the developing world, there is terrible mortality – about 100,000 deaths – among children under the age of 5,” Simpson said. “That’s because their mothers may have poor immune systems and so can’t pass on much protective immunity to their newborn.”
Icosavax’s RSV vaccine, IVX-121, is expected to enter clinical trials in 2021. It uses the stabilized prefusion F antigen DC-Cav1, licensed from the National Institute of Allergy & Infectious Diseases at the National Institutes of Health. Preclinical studies suggests IVX-121 is 10 times more effective than the DS-Cav1 antigen alone at neutralizing RSV.
“The effectiveness of IVX-121 is related to how the immune system perceives foreign threats,” Simpson said. “When the immune system see repetition, it activates. By taking a piece of the DS-Cav1 antigen and putting it on the soccer ball (putting VLPs on a 3D structure), we’re creating a repetitive array, essentially telling the immune system, ‘This is bad. Go get it.’”
Icosavax spun out of the University of Washington in early 2018, raised seed financing and began the tech transfer. Now the challenges are preparing for a clinical trial and fine-tuning the manufacturing process.
“The technology has worked as we envisioned, and we’re learning a lot from the manufacturing perspective that will be invaluable as the platform develops,” Simpson said. “We’re focusing on traditional recombinant protein scale up in a way that enables faster throughput for the next indication.”
The company raised $51 million in 2019 and boasts as chairman of the board, Tadataka (Tachi) Yamada, M.D., former CMO and CSO of Takeda Pharmaceuticals. Before joining Takeda, he was president of the Bill & Melinda Gates Foundation Global Health Program.
Read the original article on BioSpace.