Alpacas produce unique antibodies – called nanobodies – that can bind very specifically to a protein. The research team are developing nanobodies specific for the SARS-CoV-2 ‘spike’ protein, which sticks out from the surface of the virus and allows the virus to bind and enter human cells.
The team hopes that developing nanobodies against the ‘spike’ protein could be an important step towards new antibody-based ‘biologics’ therapies to treat COVID-19.
This nanobody program against COVID-19 is part of a consortium-led effort that brings together the expertise of Victorian and Australian academic and industry leaders in infectious diseases and antibody therapeutics at WEHI, the Doherty Institute, CSL, Affinity Bio, CSIRO, the Burnet Institute and the Kirby Institute.
At a glance
1- Alpacas produce unique antibodies – called nanobodies – that may offer insight into the development of new antibody-based therapies to treat COVID-19.
2- Antibody-based therapies can be used both to prevent and treat disease and are particularly useful in older people or those who are immunocompromised, who may not be able to mount a robust immune response to a vaccine.
3- Antibody-based therapies could offer one potential solution to COVID-19 and could be used alongside other treatment methods to combat this global pandemic.
Nanobodies – the building blocks for antibody-based therapies
Antibodies are key infection-fighting proteins in our immune system. An important aspect of antibodies is that they bind tightly and specifically to another protein, said Associate Professor Wai-Hong Tham, who is leading the research at WEHI.
“Antibody-based therapies – or ‘biologics’ – utilise this property of antibodies, harnessing an antibody that binds specifically to a protein involved in disease. In our case, we are looking to develop a therapy that binds to the SARS-CoV-2 virus’ ‘spike’ protein, which it uses to get into human cells. These antibodies could prevent the virus binding to the human receptor called ACE2 – stopping the COVID-19 infection cycle,” she said.
A quirk of the alpaca immune system makes alpaca antibodies a key resource in this project.
“Alpacas make unique antibodies, which are smaller than conventional antibodies. Conventional antibodies are composed of two immunoglobin – heavy chains and light chains – whereas alpacas make the majority of antibodies that lack the light chains. Nanobodies are laboratory-made antibody fragments of the heavy chain only domain that recognizes foreign proteins. These bind really specifically to their target protein and are more stable than other antibodies,” Associate Professor Tham said.
To generate nanobodies against SARS-CoV-2, a group of alpacas in regional Victoria are being immunized with a synthetic, non-infectious, part of the SARS-CoV-2 ‘spike’ protein.
“The synthetic ‘spike’ protein is not infectious and does not cause the alpacas to develop disease – but it allows the alpacas to develop nanobodies,” Associate Professor Tham said.
“We can then extract the gene sequences encoding the nanobodies and use this to produce millions of types of nanobodies in the laboratory and then select the ones that bind to the ‘spike’ protein.”
“We are now comparing these nanobodies to discover which are the most effective at binding the ‘spike’ protein and blocking the virus from entering cells. These antibodies could enable the development of new treatments against COVID-19.”
ANSTO’s Australian Synchrotron was a critical resource in the project, allowing the research team to map which parts of the ‘spike’ protein the nanobodies bound to and how this impacted the virus’ ability to bind to its human receptor.
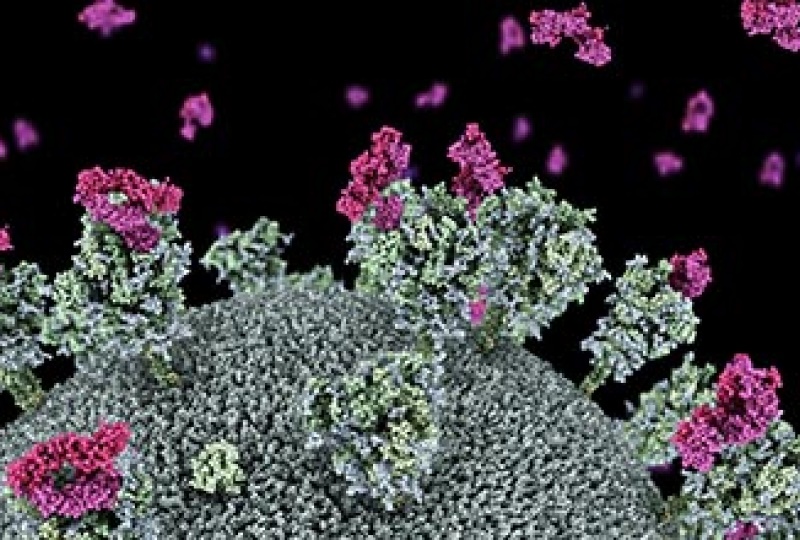
Visualization of SARS-CoV-2 virus with nanobodies (purple) attaching to the virus ‘spike’ protein.
Using antibody therapies to treat COVID-19
Antibody therapies are already in clinical use for diseases such as cancer, inflammatory and autoimmune conditions.
They can be used both to prevent and treat disease and are particularly useful in older people or those who are immunocompromised, who may not be able to mount a robust immune response to a vaccine. Associate Professor Tham said antibody-based therapies differed from vaccines.
“Vaccines elicit an immune response to produce antibodies, whereas antibody-based therapies deliver effective antibodies directly. While this means the antibody-based therapies start working straight away, they would not provide long-term protection. In contrast, a vaccine takes some time to build protective immunity, but this immunity can last for months, years, or decades.”
The research is at an early stage, but the team are hopeful it will help in the fight against COVID-19.
“We are in the early stages of this research and there are a number of steps that need to take place in developing the therapies, as well as clinical trials, before this treatment could be used in humans. But we are hopeful antibody-based therapies could offer one potential solution to COVID-19 and could be used alongside other treatment methods to combat this global pandemic,” Associate Professor Tham said.
“While we are not sure yet when these treatments for COVID-19 will be available to the public, we are working as hard as we can to make these safely available as soon as possible. I have never seen groups of people mobilizing scientifically in such a passionate and collaborative way.”
Read the original article on Walter and Eliza Hall Institute (WEHI).







