At a recent event organised by the European Alliance for Access to Safe Medicines (EAASM), EU lawmakers and stakeholders focused on nanomedicines, which are emerging as an innovative technology in the scientific field, as they help address unmet medical needs and offer alternatives for many therapeutic areas.
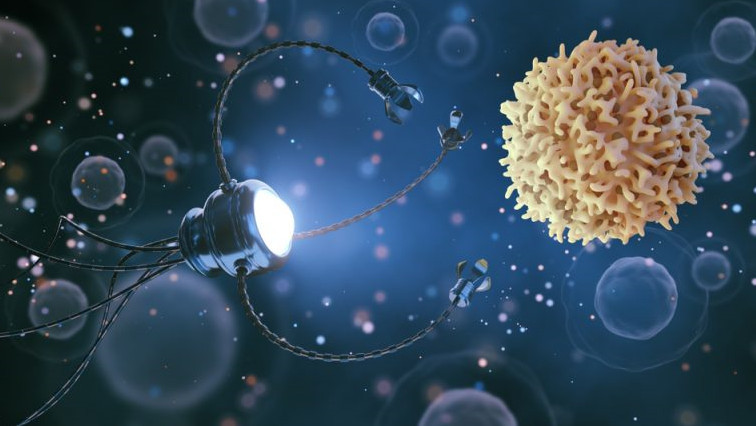
Nanomedicine uses state-of-the-art nanotechnology like nanoparticles, nanorobots or nanoelectronic biosensors for diagnosing or treating cancer, cardiovascular, and neurodegenerative diseases.
The pharma industry has mounted the pressure on the European Commission to play a more active role when it comes to nanomedicines. The EU executive recently published its new Pharmaceutical Strategy, in which the push for innovation is taking centre stage.
“Under affordability and access to medicines, there is a quite a big push for boosting medicines that basically respond to unmet needs,” Anthony Rodiadis from the European Commission’s DG SANTE commented.
However, a number of issues related to the regulatory framework raise more questions than answers while critics suggest that without an EU-centralised approach, the potential of nanomedicines will remain untapped.
In addition, at present, there is no specific regulatory pathway for follow-on nanosimilars. Given their highly complex manufacturing process, it is possible that even the slightest change from the original nanomedicine would result in a different level of efficacy.
Maria da Graça Carvalho, a Portuguese MEP from the European People’s Party (EPP), emphasised the potential of nanomedicines in delivering unmet medical needs but noted that the current regulatory framework puts severe obstacles on the process.
“We may conclude that the practical translation into treatments has not progressed as quickly as we would like to and as the enormous positive preclinical results have suggested. We are convinced that the reason for this is that we do not have a strong fit-for-purpose regulatory framework,” the centre-right EU lawmaker said.
Nanotechnology and COVID-19
Jon De Vlieger, director of business development at Lygature, a not-for-profit partnership management provider bringing together academia, industry and society, said nanomedicines are already being provided to patients saving lives every day.
He added that two of the front runner vaccines for COVID-19, Pfizer and Moderna, which the European Medicines Agency is expected to approve on 29 December and 12 January respectively, do include nanotechnology-based approaches.
“Both vaccines are based on lipid-based nanoparticles. So, it’s important to realise that it has a huge opportunity, it’s already established, but there are still some challenges that we need to solve,” he said.
There are different procedures to authorise a medicine in Europe: mainly the centralised and the de-centralised processes. In the centralised procedure, the European Medicines Agency (EMA) conducts its own scientific studies, and then the European Commission gives the green light for market authorisation. The Commission’s decision is valid in all EU member states.
On the other hand, the de-centralised procedure is used for authorising medicines in more than one EU member states in parallel. According to EMA, it can be used for medicines that do not need to be authorised via the centralised procedure and have not already been authorised in any member state.
Nanomedicines are by nature complex and things become even more complicated due to the lack of a centralised approach: currently, regulatory authorities at the member state level assess them differently.
De Vlieger presented a study on 85 different nanomedicines applications. Just two of these products were approved through the centralised procedure.
He explained that a centralised process should be the best route for nanomedicines as “it guarantees consistency in the scientific evaluation of these products,” and centralised safety monitoring.
Read the original article on EurActiv.