Notably, one of the nanoantibodies neutralized the South African variant of concern B.1.351 that has been shown to reduce the effectiveness of vaccines against the virus.
“Therapeutic options that work against the B.1.351 variant are urgently needed to counteract reduced vaccine efficacy,” writes Peter Durcan from Afrobodies Pty Ltd in Cape Town and colleagues from the Africa Health Research Institute in Durban and the MRC-University of Glasgow Centre for Virus Research.
“The antibodies described here may be a useful tool for clinicians who are treating patients infected with B.1.351 and other strains of SARS-CoV-2 for which there is currently no known highly effective treatment,” says the team.
A pre-print version of the research paper is available on the bioRxiv* server, while the article undergoes peer review.
Variants have emerged that threaten the efficacy of current vaccines
Since the COVID-19 pandemic first began in Wuhan, China, in late December 2019, the causative agent SARS-CoV-2 has infected more than 137 million people and claimed the lives of more than 2.95 million.
Vaccines protecting against SARS-SoV-2 infection have been developed at an unprecedented rate, with Phase 3 trial data demonstrating excellent efficacy in preventing COVID-19 and death.
However, since these promising results were released, SARS-CoV-2 lineages have emerged that enable the virus to escape antibody neutralization by sera from vaccinated individuals, suggesting that vaccines may be less effective against such variants.
The B.1.351 lineage is of particular concern
One variant of particular concern is the B.1.351 lineage identified in South Africa and has now become the dominant strain circulating in the country.
Sequence analysis of B.1.351 identified several amino acid differences between the spike proteins of the B.1.351 lineage and the original Wuhan isolate of SARS-CoV-2. The spike protein is the main surface structure the virus relies on to bind to and infect host cells.
These amino acid changes in the spike, together with the high prevalence of B.1.351 in the South African population, suggest that this variant may be able to evade the neutralizing antibody response that is triggered by natural infection and vaccination.
“Clinical trials have reported that at least one vaccine currently being used globally for COVID-19 prevention has a reduced efficacy in preventing COVID-19 disease mediated by infection with the B.1.351 variant,” says Durcan and colleagues.
Neutralization escape poses significant challenges
The evolution of neutralization escape mutations poses significant challenges to vaccine design and the global management of COVID-19 since no highly effective treatments for the disease are yet available.
The most successful therapeutic to date is the steroid dexamethasone, which can reduce the risk of death among patients under invasive mechanical ventilation by approximately 30%, compared with standard care.
Other chemical compounds are under investigation as treatment approaches, including repurposed antiviral drugs such as remdesivir and monoclonal antibody cocktails such as casirivimab and bamlanivimab.
“However, their development time to reach the clinic may take many years,” writes Durcan and colleagues.
An alternative is the development of biological products such as antibodies that can bind to the virus and neutralize it, says the team.
However, as is the case with vaccines, some of the neutralizing antibodies that have been developed to date are also ineffective against SARS-CoV-2 variants such as B.1.351.
Where do nanobodies come in?
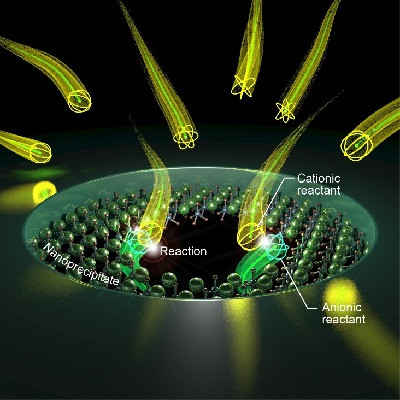
Nanobodies that have previously been raised against a range of infectious viruses, including HIV, hepatitis B, influenza, rabies, and polio have exhibited potent neutralizing activity.
Nanobodies exhibit high thermal and chemical stability and a high affinity for their target antigens. They are also able to access epitopes that are inaccessible to conventional antibodies.
“Hence, it should be possible to develop nanobodies that recognize novel epitopes that retain broad neutralizing activity,” says Durcan and the team.
What did the researchers do?
The team set out to investigate recombinant alpaca antibodies as novel therapeutics to neutralize SARS-CoV-2 variants such as B.1.351.
An alpaca was immunized with recombinant subunit 1 of the SARS-CoV-2 spike protein and the animal’s serum was tested 2, 4 and 8 weeks later for neutralizing activity against the SARS-CoV-2 variant CVR-GLA-1.
Eight different nanobody sequences that bound to the recombinant S1 protein were isolated, namely A1, A2, B1, B7, C3, C9, C12, and H4. When the eight nanobodies were tested against the CVR-GLA-1 variant, four (A1, A2, C3 & C9) displayed potent neutralizing activity.
Three of the nanobodies – A1, C3, and C9 – also potently neutralized the B.1.1 variant, but nanobodies C3 and C9 showed no neutralization activity against B.1.351. However, nanobody A1 displayed potent neutralizing activity against both B.1.1 and the B.1.351 variant.
A1 may target a conserved epitope
“These data may indicate that the A1 nanobody targets an epitope that is conserved between variants,” say the researchers.
This epitope may not be under selective pressure in the general population as it is inaccessible to conventional antibodies, they add.
“Due to the lack of current treatment options available to clinicians for the treatment of COVID-19, the nanobodies reported here may be a useful tool for them to use in order to save patient lives,” concludes the team.
Read the original article on Medical News.