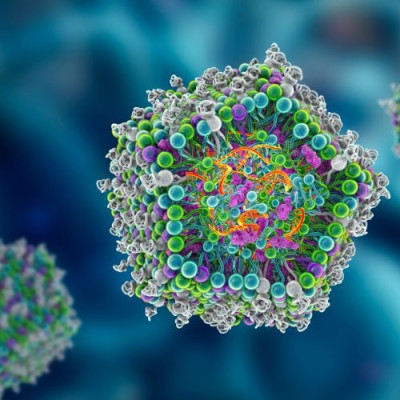
Traditionally used to treat a variety of conditions, including cancer and autoimmune and inflammatory diseases, nanobodies are smaller components of conventional antibodies — a vital element of the body’s immune system that defends against disease-causing viruses or bacteria.
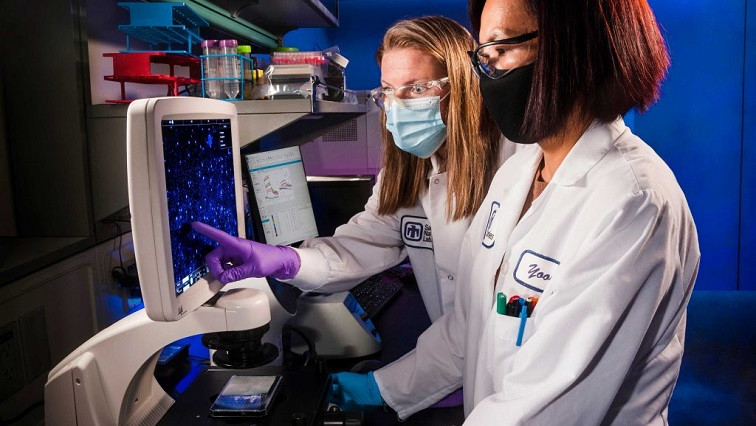
After screening a large, diverse library of synthetic nanobodies, Sandia researchers identified and evaluated several potent nanobodies that can protect against COVID-19. The scientists now aim to replicate this method to defend against current and future biological threats.
“The coronavirus pandemic has made evident the need for a broad range of preventive and therapeutic strategies to control diseases associated with novel viruses,” said Craig Tewell, director of Sandia’s Chemical, Biological, Radiological and Nuclear Defense and Energy Technologies Center.
With a rich history of biodefense research, Sandia helps protect the nation and the world from threats presented by bioterrorism and naturally occurring diseases, Craig said.
“With a deep understanding of how infectious disease develops and spreads, as well as how the immune system defends from infection,” Craig said, “our researchers are in a unique position to advance the creation of a wide array of disease-fighting tools, including nanobodies.”
Virologist Brooke Harmon leads Sandia’s nanobody research, a new and growing area of bioscience.
“Vaccines are very good at preventing infection, but they can take a long time to be developed and move through the regulatory process,” Brooke said. “We saw a critical need to create effective therapies that can be rapidly developed and deployed.”
Once the protein sequence, or genetic coding, of a virus has been identified, Sandia researchers have shown they can produce a nanobody-based countermeasure within 90 days. The method has not yet been tested on humans. Speeding up the discovery of neutralizing antibodies could reduce the impact of future viral outbreaks.
“Under current practice, virologists rely upon patients’ blood samples to build an antibody library that we can then screen for potential treatments. This means we have to wait, either for people to become infected or for those who are vaccinated to build an immune response,” Brooke said. “Sandia’s new method is more forward-thinking. Because we have already built a highly diverse, proprietary library, we can begin to screen for extremely potent neutralizing nanobodies as soon as the genetic coding of a virus has been identified.”
Nanobodies’ diverse attributes
Neutralizing nanobodies represents an attractive strategy, Brooke said, due to their ability to work effectively against an entire family of viruses or variants.
“We can take advantage of the fact that virus families tend to interact with immune response in the same way,” Brooke said. “This makes our treatments rapidly adaptable to all variants of a virus.”
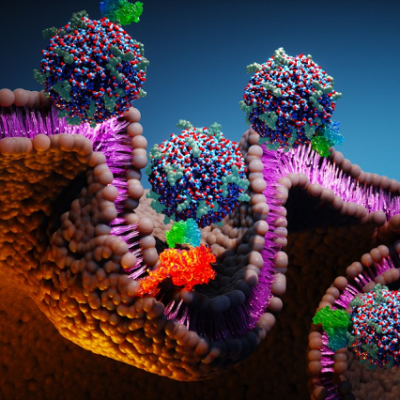
Nanobodies are modular, meaning they can be combined with other nanobodies to increase their ability to bind to the virus or target specific tissues. Nanobodies can also be produced as smaller versions of conventional antibodies with the ability to engage the immune response.
Additionally, due to the small size of the nanobodies, they can be released into the blood and penetrate tissues more thoroughly than conventional antibodies. Nanobody therapies can also target an infection site directly, decreasing the dose needed and increasing efficacy.
Nanobodies can also be administered via aerosol, so they can be given to a patient orally or in an inhalable form. Conventional antibody treatments are less versatile and must be received through injection only.
“All of these qualities and features of nanobodies make nanobody therapies more effective than current solutions. These treatments are also easier and cheaper to manufacture,” Brooke said, “making Sandia’s method for developing and characterizing novel neutralizing antibodies an invaluable addition to the toolset for combatting the COVID-19 pandemic and future health crises.”
Read the original article on Sandia National Laboratories.