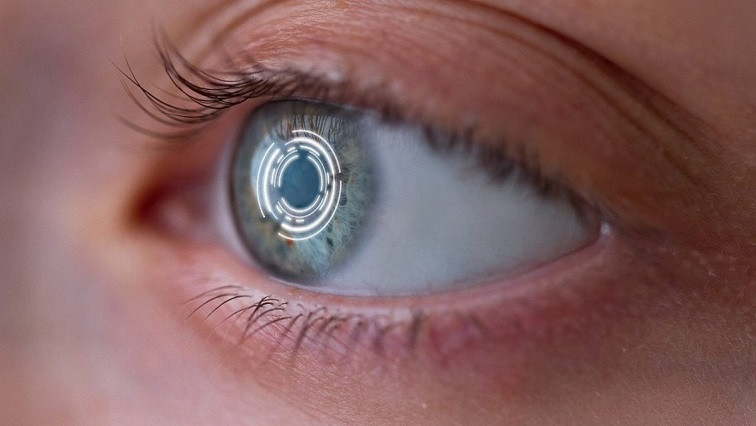
Taylor hopes the tiny electrodes could someday be implanted into the eye to restore sight in people with macular degeneration or other vision disorders.
The new work provides experimental evidence supporting a hunch his team has been pursuing for years, that neurons, which themselves are fractals, will connect better to a fractal-patterned electrode than they do to more traditionally shaped electrodes, allowing better signal transmission between the implant and the brain.
Taylor and his colleagues report their findings in a paper published April 6 in the journal PLOS One.
“The reason I'm so excited is that this paper is three years of data that explores what happens when these retinal cells interact with a fractal electrode,” he said.
Neural implants have a futuristic sheen, but they’re already being used to help people with conditions ranging from Parkinson’s disease to spinal cord injury. A chip that stimulates a particular spot within the brain can help reduce tremors or even restore the ability to move, speak or see.
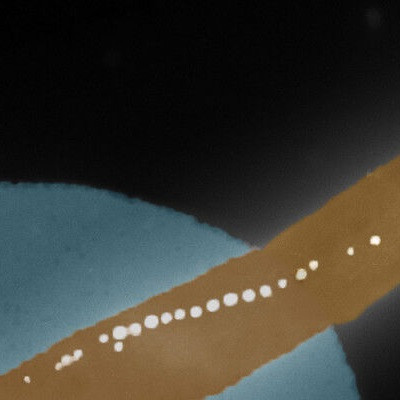
To successfully send signals to the brain or the eye, an implanted electrode needs to be able to connect to a network of existing neurons. Neurons naturally grow in a tree-like fractal pattern, leading to ever-finer branches.
Most electronics aren’t shaped like that; they’re designed for use inside machines, not living things. Instead, Taylor thought, why not coax the neurons to connect to an electrode in a pattern that fits their tendency?
“You want neurons to get attached to be stimulated; that’s the ultimate goal in designing any sort of electrode,” said Saba Moslehi, a postdoctoral researcher in Taylor’s lab. “And when two objects have very similar characteristics, they’ll have more of a tendency to interact compared to objects that have completely different characteristics.”
Taylor, a physicist who specializes in fractals, submitted the idea to a life sciences research competition in 2014. To his surprise, it beat out almost a thousand competing ideas. And since then, with help from UO professors Benjamin Aleman and Cris Niell and collaborators at Lund University in Sweden, his group has been exploring its potential.
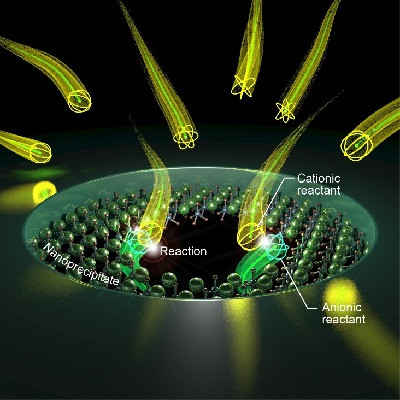
In past studies, they performed computer simulations which suggested the fractal-patterned electrodes would be more effective than traditional electrode shapes. Then, to test the idea experimentally, the UO team used electrodes made from smooth silicon chips with branches made of carbon nanotubes patterned on the chip surface.
Neurons prefer to attach to the textured nanotubes, so researchers can control where neurons will attach to the electrode by modifying the nanotube map on its surface.
Moslehi, along doctoral students Conor Rowland and Julian Smith, used facilities at the UO’s Center for Advanced Materials Characterization in Oregon to create silicon-based with carbon nanotubes arranged in a fractal pattern shaped like a repeating letter H.
For comparison, they also made chips with the nanotubes arranged in parallel lines, a design one might see on a commercially available electrode chip.
Then, they tracked how mouse retinal neurons grew on the chips, using cells cultured in a petri dish.
Neurons attached more prevalently to the textured fractal branches than to the smooth gaps between the branches, the experiment showed. And glia, important support cells for neurons, packed tightly into the smooth gaps. The fractal design was the most effective at this ‘herding’ of neurons and glia.
“The really clever thing is that we've managed to put the glial cells in the gaps,” Taylor said. “Glia are the life support system of the neurons, and we need to induce favorable interactions with both the neurons and the glial cells.”
The work is still early-stage, Taylor emphasized. Running trials in animals will take additional engineering and safety tests. But eventually, the researchers hope their design will turn into a real-world device that can help people with vision loss.
And the fractal patterned, bio-inspired electrodes might have uses in brain implant research beyond the bionic eye.
“I think this could help not just the system we tested, but implants in other parts of the nervous system as well,” Moslehi said. “I hope to see more researchers moving towards using fractal electrodes rather than commercial patterns.”
Read the original article on University of Oregon.