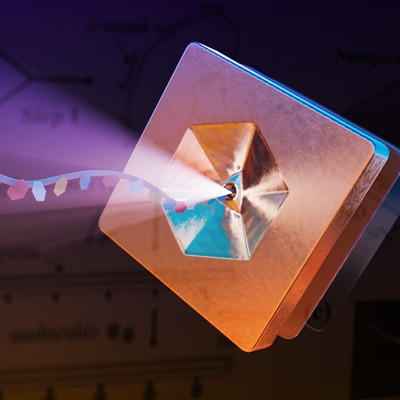
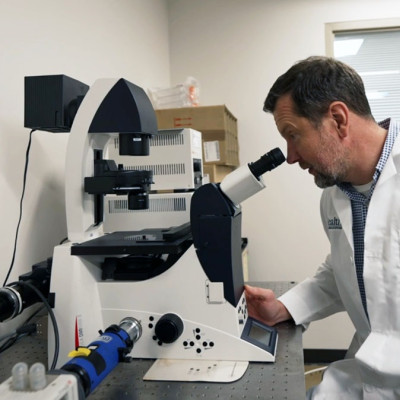
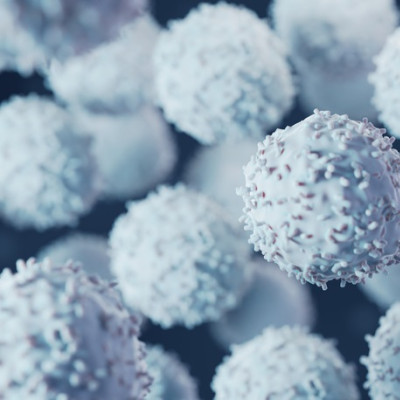
Nanomedicine is a complex and diverse term, encompassing the use of nanomaterials for diagnosis, control, prevention, and treatment of diseases. Whilst there is scientific agreement around its broad definition, an underlying debate exists around its size-based cut-off point.
The applications of nanotechnology in pharma have served to overcome significant limitations presented by standard small molecule drugs regarding their solubility, bioavailability, and pharmacokinetics. Nanomedicine is not limited to nanopharmaceuticals but also includes devices, such as lateral flow tests that use gold nanoparticles to detect specific biomarkers or the use of nanofibers as scaffolds for tissue regeneration.
Since 1989, 78 medicines have received approval on a global scale with 66 nanodrugs being approved by the FDA and 31 by the EMA. With the emergency use authorisation and success of the Pfizer and Moderna SARS-CoV-2 vaccines, the applications of nanotechnology are set to take off. The key to the successful development of nanomedicines relies on an in-depth understanding of their toxicity and potential adverse effects.However, navigating market challenges to ensure the access and uptake of nanomedicine will be equally important and renewed conversations around regulation, distribution, availability, and reimbursement will be critical.
Regulating the unregulatable?
Pharmaceutical companies face some of the heaviest regulations as an industry, given the importance of comprehensive and harmonised guidance and rules to ensure safety and efficacy when bringing treatments to the market. Regulation, as we know it, tends to rely on the categorisation and classification of products into relatively clear groups. By putting products into different boxes (e.g. chemical drugs versus biologics), regulators have managed to develop very clear processes that are tailored to the unique characteristics of different treatment types.
However, the categorisation of nanomedicines is not that straightforward. It is the complex nature of nanomedicines that makes it hard to agree on all-encompassing definitions and classification that capture their diverse nature. As a result, tying nanomedicines into the existing regulatory processes has been challenging. For example, some countries and regions consider nanomedicines as medicinal products, whilst others have opted to classify them as medical devices. In addition, existing safety data requirements are not always appropriate for the analysis of nanomedicines. Not only does this create a series of obstacles to manufacturers looking for market authorisation, but also raises questions around the safety monitoring after its marketisation. The result? Regulatory uncertainty across the world.
In the EU, a wide range of stakeholders (including policymakers) have called for new regulatory processes to be set up to avoid diverging approaches between Member States in light of the revision of the general pharmaceutical legislation.
Giving the EU a chance to set a precedent
In November 2021, the European Parliament adopted an own-initiative resolution on a pharmaceutical strategy for Europe, guiding the European Commission ahead of its proposal on the update of EU pharmaceutical legislation by the end of 2022. In the adopted text, Members of the European Parliament called on the Commission to build a “centralised approval framework for nanomedicines”.
The core issue experienced at the EU level is that regulatory approvals for these medicines are currently decided on an ad-hoc basis by product category, with both nanomedicines and their follow-on products, nanosimilars, majorly relying on non-centralised procedures.
Despite the noise that has been made around this – mainly led by the European Alliance for Access to Safe Medicines, with a wide range of policymaker and academic support – there are still a lot of questions in the air.
The EC’s position on this topic has never been very clear. In 2020, Commissioner Kyriakides insisted that the legal framework for pharmaceuticals applies for the approval of nanomedicines and nanosimilars, and therefore there is no need to revise the pharmaceutical legislation for this. Less than one year later, however, her position on this topic was much more nuanced, stating that the revision of the legislation would assess its performance regarding innovative scientific and technological developments, including nanomedicines. Whilst there is an overall feeling that the tide might be changing, exerting continuous pressure on this topic will be essential.
Greater clarity around nanomedicines in the revised pharmaceutical legislation should not only be regarded as a necessary next step to ensure patient safety and promote innovation by the European Union, but also as an opportunity for them to lead on this conversation at the global level. Whilst countries like the United States have made major progress on the topic, the FDA and a wide range of other agencies still use a case-by-case approach under the traditional framework of benefit/risk analysis. The European Union has the chance to set a precedent and show that tailored regulatory processes for nanomedicines are possible, opening the door for more and better innovation around the world.
Read the original article on PMLiVE.