Brain tumors are notoriously hard to treat. One reason is the challenge posed by the blood-brain barrier, a network of blood vessels and tissue with closely spaced cells. The barrier forms a tight seal to protect the brain from harmful substances, but it also prevents most drugs from getting to brain tissue. This severely limits therapies that can be used for brain tumors.
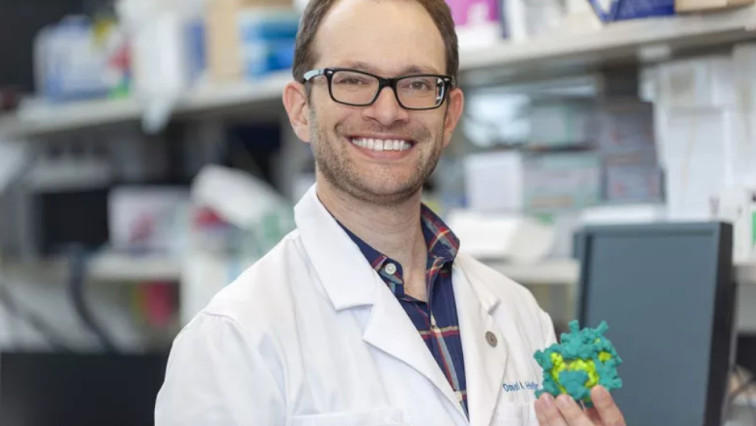
Now, a Memorial Sloan Kettering Cancer Center (MSK) team led by Sloan Kettering Institute biomedical engineer Daniel Heller, PhD, in collaboration with Praveen Raju, MD, PhD, a pediatric neurologist at Mount Sinai Medical Center, may have found a way to carry drugs across the blood-brain barrier using nanoparticles — tiny objects with diameters one-thousandth that of a human hair. The researchers showed that this approach could work in mouse models of medulloblastoma, the most common malignant (cancerous) pediatric brain tumor.
Here, Dr. Heller explains how this method, reported March 2 in Nature Materials, could potentially improve treatment for medulloblastoma, other brain tumors, and other brain diseases.
How are nanoparticles used to target tumors across the blood-brain barrier?
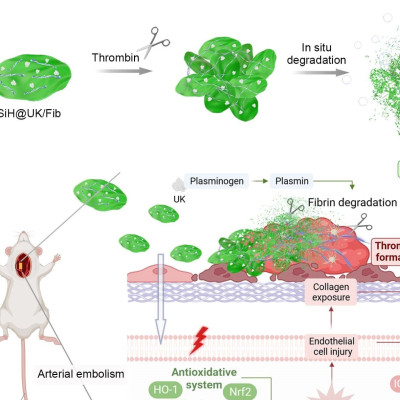
In 2016, my laboratory found that a protein called P-selectin is an especially good target on cancer blood vessels for steering nanoparticles, loaded with drugs, to tumors. P-selectin is abundant in blood vessels that feed tumors. We found a substance that has a natural affinity for P-selectin. It’s called fucoidan, a polysaccharide (a chain of sugar molecules) that is widely available and extracted from brown seaweed from the Sea of Japan. Fucoidan binds to P-selectin.
In the 2016 study, we filled fucoidan nanoparticles with different cancer drugs and showed that the nanoparticles selectively attached to cancer sites, including metastatic tumors in the lungs of mice. This showed the promise of targeting P-selectin to treat cancer.
How does targeting P-selectin get drugs across the blood-brain barrier?
The blood vessels in the blood-brain barrier are lined with a layer of cells that are packed very close together. We discovered that when the nanoparticle binds to P-selectin, it triggers a process called transcytosis, a mechanism that shuttles a particle across the cells lining the blood vessel wall. This allows something inside the blood vessel to pass through the vessel wall to reach the surrounding brain tissue. We found we could exploit this natural mechanism to get drug-loaded nanoparticles across the blood-brain barrier, which has been very difficult to achieve.
This could be an important step in improving treatment of brain tumors and other brain diseases. People have tried different ways to disrupt the barrier, like using ultrasound to poke tiny holes. For many reasons that are probably obvious, these methods carry risks. But now we may have a way to get around some of these risks.
How did you end up testing this approach on medulloblastoma?
A pediatric oncology fellow working in our lab, Hiro Kiguchi, MD, was studying the use of these nanoparticles for pediatric cancers. He presented our work to scientists and physicians in MSK’s pediatrics department, and Praveen, who was working here at Memorial Sloan Kettering and Weill Cornell Medicine at the time, asked: “Could you could get these nanoparticles across the blood-brain barrier?” I was skeptical because even though nanoparticles are small, they still are bigger than drugs or proteins, and the barrier is so tight.
But it turned out Praveen had developed a mouse model for medulloblastoma. This was ideal for testing our technology because the blood-brain barrier is intact in this model, unlike many other brain tumor models, which have leaky barriers. We collaborated with Praveen, who is a co-corresponding author on the study, to put this nanoparticle approach to the hardest test.
How did you demonstrate that the nanoparticles can reach the medulloblastoma in mice?
We loaded the nanoparticles with a drug called vismodegib, which targets the Sonic hedgehog signaling pathway. Sonic hedgehog proteins play an important role in promoting cancers. Vismodegib has already been approved for treating basal-cell carcinoma, the most common skin cancer, and the drug had been tested for medulloblastoma and other cancers driven by Sonic hedgehog proteins. However, this drug resulted in significant bone-related side effects when it was tried in pediatric medulloblastoma patients.
We found this side effect does not occur when we put the drug into nanoparticles. We injected vismodegib-loaded nanoparticles into the tail vein of the medulloblastoma mouse models and let it circulate to see if it passed through the barrier. Using special imaging, we could see the particles accumulating at the site of the medulloblastoma tumors, where P-selectin is prominent, and not in normal brain regions or other parts of the body. Daniel Tylawsky, a PhD student in our laboratory, discovered that particles that target P-selectin use the transcytosis transport route to cross the blood vessels to reach the tumors.
Using Radiation To Increase Levels of P-Selectin
One key to making this treatment effective is using radiation, which is a standard therapy for both children and adults with brain tumors. Radiotherapy boosts levels of P-selectin in tumors. This means we can direct radiation to give the nanoparticles more P-selectin to grab onto in the tumor so more nanoparticles, and their drug cargo, will end up there. In the case of medulloblastoma, we could give the radiotherapy to the specific location in the brain before injecting the drug into the vein. There are many cases where we don’t want drugs to go to other parts of the brain even if we get them across the barrier, so using radiation allows us to focus a drug to the target area.
What’s Next for Treating Diseases Beyond the Blood-Brain Barrier?
1: Test the technology in people.
We know fucoidan is safe. You can buy it at a health food store, and some people claim it boosts immune function and reduces inflammation. Nanoparticle-based fucoidan therapy would not necessarily replace surgery, which is still the standard treatment for medulloblastoma. But it could improve the effectiveness of many classes of cancer drugs to prevent the cancer from returning, allow the use of lower doses of radiation therapy to the brain, and also reduce many drug side effects.
2: Use therapies in the brain cancers that have never been tried before.
Currently, the few drugs used to treat brain tumors are those that get through the blood-brain barrier. But now, we may have a much wider range of drugs that can reach brain tumors effectively. From our studies so far, it seems that it doesn’t matter what drug you put inside the particle; we can get it across the barrier.
3: Treat other brain cancers, brain metastases, and brain diseases.
Although this approach first could be used against medulloblastoma, it has broader potential applications. Most brain tumors occur in adults, so if the therapy works against other brain malignancies, including glioblastoma or brain metastases, it could benefit many people. We also could use the approach to deliver drugs to treat noncancerous brain diseases.
Read the original article on Memorial Sloan Kettering Cancer Center (MSKCC).