Plastics are among the most ubiquitous manmade materials— we wear them, build with them, play with them, ship goods in them, and then we throw them into the waste stream. Ultimately, they can break down into tiny particles that get into our food supply, and we end up eating them.
These particles can range from about the size of pollen (microplastics) down to a fraction of the size of a virus (nanoplastics), and they have penetrated water supplies, agricultural soil beds, and natural and domestic food chains.
Knowledge of the effects of ingesting microplastics and nanoplastics has been limited by their ubiquitous nature—making it difficult to find populations of unaffected individuals to act as control groups—and the lack of relevant laboratory models for studying the particles’ effects on cells. In a study published in Nanomedicine, researchers at Tufts University School of Engineering have found potential inflammatory effects of plastic particles using human intestinal organoids — small bundles of tissue made from a mix of human cells obtained from biopsies that mimic the complexity of an actual intestinal environment.
Notably, the researchers found that higher concentrations of plastic particles triggered the secretion of inflammatory molecules linked to human inflammatory bowel disease (IBD).
Earlier clinical studies have found plastics accumulated in different tissues of living organisms, including the digestive tract, blood, liver, pancreas, heart, and even the brain. The most likely first point of entry is through the intestine. Studies on rats and other animals have found that while microplastics and nanoplastics may accumulate in the intestine and other tissues, there are conflicting results on toxic effects or inflammation, which may depend on particle size, length of exposure, and pre-existing conditions. Controversy remains as to whether there are any toxicological effects on humans, as results in animal studies don’t always track with human outcomes.
“We know that particulate plastic is everywhere in the environment, and it has been found in human intestines and other tissues, like blood, and even in the brain and placenta,” said Ying Chen, research assistant professor in biomedical engineering at Tufts University and co-lead author of the study. “The use of organoids allows us to study in detail the mechanisms of absorption and potential pathways to disease in a way that could help us make sense of the variable results in the literature up until now and have a more direct tissue model for potential effects of plastic particles on humans.”
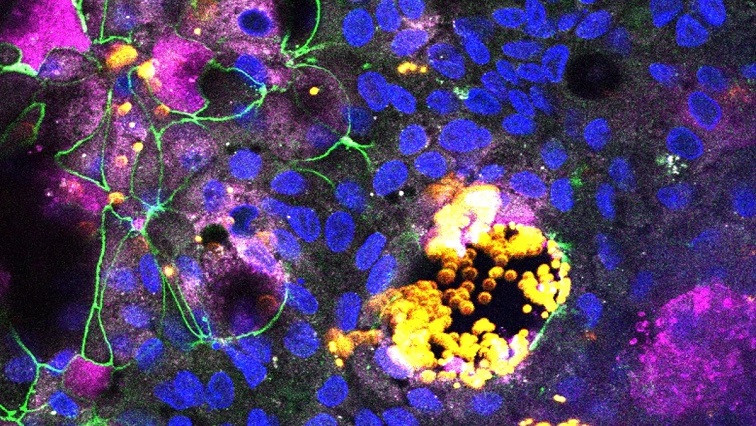
To create a physiologically relevant intestinal model, Chen and her team started with stem cells derived from organoids and coaxed them to differentiate into the various cells found in the native intestinal wall, aiming for a similar cell ratio to that in the intestine but grown in a flat layer. The cells have different and important roles including absorption, mucus secretion, hormone production, and inflammatory and other immune responses.
“It’s a significant step up from simpler cell models that often included only one or a few cell types, some of which were derived from cancer cells that might not demonstrate natural responses,” said Chen. They were able to change the mix of cells in the intestine-like organoid layer to see how it affected the response to plastic particles, which were specially modified to glow fluorescently for easy tracking.
Different cells were found to absorb different sizes of particles. Epithelial cells that normally line the inside of the intestine would absorb the tiniest nanoparticles, while microfold or “M” cells would absorb and transport larger microparticles into the intestinal tissue. The researchers also found that damage caused by plastic particles to the model intestinal lining occurred only when M cells were present and at higher concentrations of particles. Damage to the cell layer may imply the potential for generating intestinal lesions.
Notably, the researchers also observed that higher concentrations of plastic nanoparticles triggered the organoid layer to release inflammatory cytokines—molecules that are a part of the normal immune response, but may relate to diseases including Inflammatory Bowel Disease (IBD) when they are set off balance. This effect was also dependent on the presence of M cells, which suggests those cells play a critical role in mediating potential damage to the intestine by plastic microparticles. More research will have to be done to clarify the impact of concentration, chemistry and surface features of plastic particles on M cell functions, said Ying.
“The results in this study suggest that using human cell organoids could be an effective means to better understand the potential toxicity of microplastics and nanoplastics, and environmental particles in general,” said David Kaplan, Stern Family Professor of Engineering at Tufts and a pioneer in tissue engineering and the development of laboratory test models that mimic real biological tissues. “Since these small particles can also be sinks or carriers for chemicals and other contaminants in the environment, this amplifies the potential impact from the studies.”
Kaplan adds, “In fact, organoids can be grown to model many other human organs, including the stomach, kidneys, heart, pancreas, liver, and brain, which could enable us to explore effects of environmental contaminants throughout the body.”
Read the original article on Tufts University.