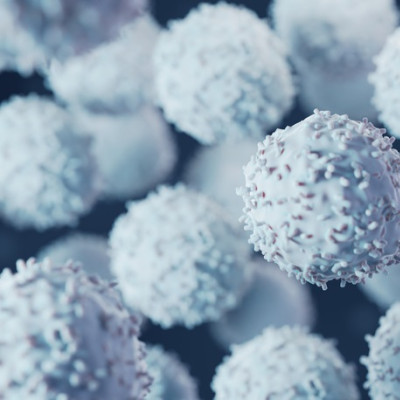
Macrophages are little cells vital to the immune system and could possibly inform cell-based therapies for a variety of medical conditions. However, realizing the full potential of macrophage therapies relies on being able to see what these cellular allies are doing inside our bodies, and a team of Penn State researchers may have developed a way to watch them do their thing.
In a study published in the journal Small, the Penn State researchers report a novel ultrasound imaging technique to view macrophages continuously in mammal tissue, with potential for human application in the future.
"A macrophage is a type of immune cell that is important in nearly every function of the immune system, from detecting and clearing pathogens to wound healing,” said corresponding author Scott Medina, the William and Wendy Korb Early Career Associate Professor of Biomedical Engineering. “It is a component of the immune system that really bridges the two types of immunity: innate immunity, which responds to things very quickly but in a not very precise way, and adaptive immunity, which is much slower to come online but responds in a much more precise way.”
Macrophages regulate these two arms of the human immune response and help our body with functions such as fighting infections and tissue regeneration. On the flip side, they also help mediate inflammation related to injuries and diseases such as diabetes and rheumatoid arthritis. According to Medina, these cells could be harnessed and applied in therapies that would help patients with conditions such as cancer, autoimmune disorders, infections and damaged tissue. Such therapies would involve isolating, modifying, and/or engineering macrophages to enhance their properties to combat disease, control immune responses and promote tissue repair.
"If we could visualize what these cells are doing in the body, in real-time, then we could learn a lot about just how diseases progress and how healing happens," Medina said. “This would give us a view of what the cells are doing in the body because right now, we're really limited to taking the cells out of the body and seeing what they do in a petri dish, which is not going to be the same behavior that we see in the body."
The researchers turned to ultrasound imaging, a common technique to see the body’s internal tissues. However, with ultrasound alone, macrophages blend in with their fellow cells.
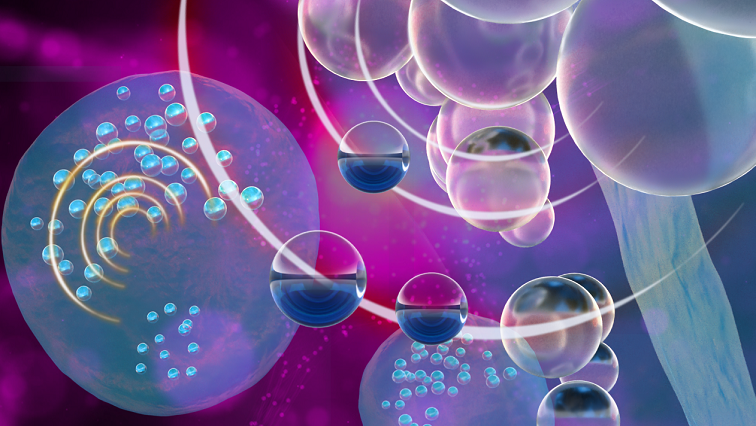
"Macrophages are basically invisible during ultrasound imaging because you can't distinguish where the cells are relative to all the other cells that are in our tissue,” Medina said. “They all behave the same so you cannot really see specific cells. We had to create what is called a contrast agent, something that our cells of interest could be labeled with that would then provide some image contrast that would be different from the background. And that is where these nanoemulsions came in.”
Many home cooks know emulsions as a mixture of oil droplets suspended in a liquid such as vinegar or water to make salad dressing; a nanoemulsion is when those oil droplets are tiny, mere nanometers in diameter.
The researchers used nanoemulsions to create more resilient bubbles. Gas bubbles reflect an ultrasound’s soundwaves very efficiently; however, if someone injects bubbles into a patient’s body, they do not work very well because they burst relatively quickly.
“We needed a way to basically get bubbles to form when we want them to form right at the time of imaging and not before, and also for these bubbles to persist as long as possible,” said Inhye Kim, post-doctoral fellow in biomedical engineering and lead author of the study.
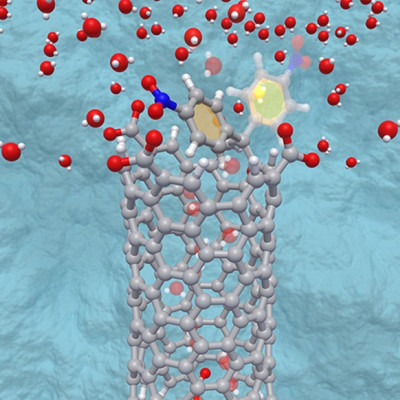
The researchers introduced nanoemulsion droplets to the cells, which internalized them. Under ultrasound, the droplets then went through a phase change, turning into a gas and, therefore, a bubble. The pressure from the ultrasound waves facilitated this change, pushing and pulling on the droplet as the wave oscillates and uses pressure to force the droplet to boil, making it vaporize and turn into a gas bubble.
“It is similar to how water will boil at a lower temperature at a higher elevation, in say Colorado, because there is less pressure preventing it from boiling,” Medina said. “We are using the pressure that we're applying on that droplet through ultrasound to effectively get it to boil when we want it to boil so then it vaporizes and causes the formation of this gas bubble.”
They tested this novel technique in a porcine tissue sample and found that the imaging of the macrophages worked. The approach allows researchers to see what immune cells are doing in the body in a continuous fashion, enabling a better understanding of how the immune system is regulated and what its role is in fighting diseases, Medina said. Beyond that, Kim noted, it can also help with developing better immune cell therapies for patients in the future.
"For example, for a patient with a tumor, this research could enable the engineering of a macrophage cell therapy that is more effective and has fewer and less serious side effects,” Kim said.
Next steps in the research include exploring the possibility of using this technique for other types of immune cell visualization within the human body, or to monitor buildup of plaque within arteries. In addition, the researchers are seeking collaborators to advance the technique.
“We are hoping to work with others in immunology research that have particular interests and might find this technology useful, so we are definitely open to further collaborations and applications,” Medina said.
Read the original article on Pennsylvania State University.