A new therapy involving laser light and sugar-coated gold nanoparticles can rapidly destroy slimy bacterial accumulations called "biofilms" that cause tooth decay and infect wounds—all without needing antibiotics.
This is the promise by a team of researchers led from the University of Pennsylvania, who have demonstrated the potential of the treatment in studies involving mice and rats.
The technique, which has been shown to outperform both a common antimicrobial and an antiseptic, could have widespread applications.
It is estimated that millions of people in the USA suffer from infected wounds each year, while tooth decay affects nearly half of the world's population.
The concept of a biofilm will be familiar to anyone who has ever slipped on a slime-covered rock while trying to ford a steam. This off-putting gunk is effectively a city of microbes, all stuck together and coated in a glue-like secretion.
Biofilms are even more of a problem in the human body, forming in open wounds and delaying the healing process—and gathering on teeth in decay-causing plaques, which can lead to painful cavities.
The challenge with these films is that slime that helps hold them together also shields the bacteria, protecting it from attacks by, for example, antibiotics.
"With this platform, you can bust biofilms without surgically [cleaning] infections, which can be necessary when using antibiotics," said Luisa Russell of the National Institute of Biomedical Imaging and Bioengineering in a statement.
"Plus, this method could treat patients if they are allergic to antibiotics, or are infected by strains that are resistant to medication. "The fact that this method is antibiotic-free is a huge strength."
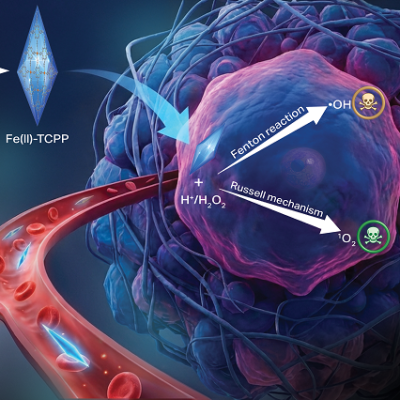
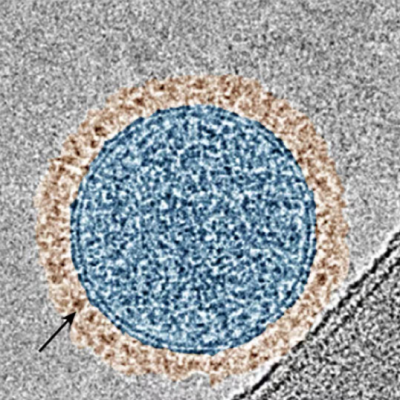
In their study, biomedical engineer professor Maryam Hajfathalian and her colleagues created nanoscopic tools by encasing gold spheres in larger gold cages.
When light is shone on these special combination particles, they emit ultrasound. This can be recorded and used to reconstruct an image of where the particles are located.
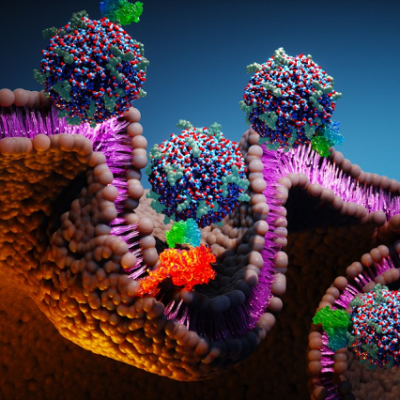
And by coating the gold-in-gold-cages with dextran—a type of sugar commonly used to build biofilms—the team were able to ensure the particles end up where the bacteria are.
In this way, the team developed a tool to image biofilms, which can be difficult to identify. However, the design of the particles allowed them to go one step further.
When a laser is shone on the gold nanoparticles, they also turn the light energy into heat—which kills the bacteria. This is a technique known as "photothermal therapy."
Gold is an ideal substance for photothermal therapy, not only because it readily converts light into heat and ultrasound, but also because it is non-toxic.
To test the potential of their photothermal therapy, the team applied their nanoparticles both to teeth, pulled from rats' jaws, that had been coated in Streptococcus mutans; as well as to open wounds, on mice, that had been infected with Staphylococcus aureus.
In the experiments on the teeth, shining light on the particles allowed the team to clearly image where the biofilms had accumulated.
When a near-infrared laser was used, the particles succeeded in killing off 100 percent of the plaque.
In contrast, treatment with the topical antiseptic chlorhexidine—a common ingredient in mouthwash—was found to have little effect on the bacteria infecting the teeth.
"The treatment method is especially fast for the oral infection," noted Hajfathalian in a statement.
"We applied the laser for one minute, but really in about 30 seconds we're killing basically all of the bacteria.
In the tests involving mice with open wounds, the team found that the photothermal therapy significantly outperformed gentamicin, an antimicrobial agent used for comparison.
At the same time, the team were able to record a 36 F (20 C) increase in temperature in the treated biofilm—with no apparent effect on the surrounding tissue.
"I think it's important to see how inexpensive, straightforward and fast this process is," Hajfathalian said. In fact, she explained, a dose of the nanoparticles sufficient to cause 'dramatic' decreases in bacteria numbers costs only $0.20 to produce.
The nanoparticles, she told Newsweek, "could be included in a variety of daily oral and skin health maintenance products—such as mouth rinses, gel strips, and photothermal bandages."
To prevent bacteria developing greater resistance to antibiotics, the use of these drugs must be controlled carefully.
"Since we are limited in using antibiotics, we need novel treatments like this as a replacement," Hajfathalian explained.
With their initial study complete, the researchers are now planning to explore whether their nanoparticle-based therapy could help to prevent cavities in teeth, or speed up the healing of treated wounds in practice.
The team are also looking to explore whether the concept might be adapted against other biofilm infections—such as those in catheters, gastrointestinal tracts, heart valves, lungs and prosthetic joints.
The full findings of the study were published in The Journal of Clinical Investigation.
Read the original article on Newsweek.