When cancer breaches the brain, it can be difficult for treatment to follow.
Brain metastases, as these secondary tumors are called, most commonly arise from solid tumors like breast, lung and colon cancer and are often associated with a poor prognosis. In some cases, patients may not even know they have cancer until the secondary tumors cause symptoms, such as seizures. The difficulty of treating brain metastases stems in part from the blood-brain barrier, a near-impenetrable membrane that separates the brain from the rest of the body.
Now, a team of researchers at Sylvester Comprehensive Cancer Center, part of the University of Miami Miller School of Medicine, has developed a nanoparticle that could one day be used to treat brain metastases, with the added benefit of treating the primary tumor at the same time.
The researchers, led by Shanta Dhar, Ph.D., assistant director of technology and innovation at Sylvester and an associate professor of biochemistry and molecular biology at the Miller School, described the new method in a paper published May 6 in the journal Proceedings of the National Academy of Sciences (PNAS). By loading the particle with two mitochondria-targeted prodrugs, the researchers showed that their method could shrink breast and brain tumors in laboratory studies.
“I always say nanomedicine is the future, but of course we have already been in that future,” said Dr. Dhar, referring to commercially available COVID-19 vaccines, which use nanoparticles in their formulation. “Nanomedicine is definitely also the future for cancer therapeutics.”
Taking Aim at Cancer Metabolism
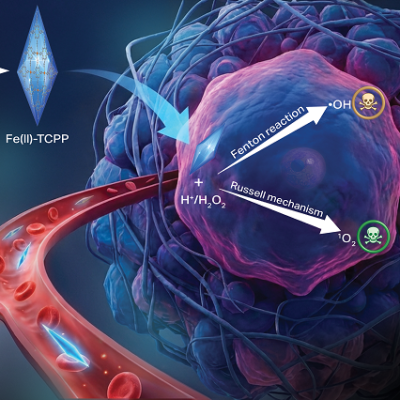
The new method uses a nanoparticle made of a biodegradable polymer developed by Dr. Dhar’s team. The researchers couple the polymer with two drugs also developed in her lab that take aim at cancer’s energy sources. Cancer cells often have a different form of metabolism than healthy cells and stifling their metabolism can be an effective way to kill tumors without harming other tissues.
One of these drugs is a modified version of cisplatin. The classic chemotherapy drug kills cancer cells by damaging DNA in rapidly growing cells, effectively halting their growth. But tumor cells can repair their DNA, sometimes leading to cisplatin resistance.
Dr. Dhar’s team modified the drug to shift its target from nuclear DNA—the DNA that makes up our chromosomes and genome—to mitochondrial DNA. Mitochondria are our cells’ energy sources and contain their own, much smaller genomes. For cancer therapeutic purposes, they don’t have the same DNA-repair machinery that our larger genomes do.
Because cancer cells can switch between different sources to sustain their growth and proliferation, the researchers combined their modified cisplatin (Platin-M) that attacks oxidative phosphorylation with another drug they developed, Mito-DCA. That drug specifically targets mitochondrial kinase and inhibits glycolysis.
Getting to the Brain
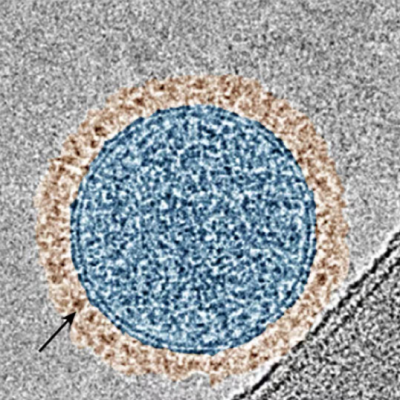
It was a long route to develop a nanoparticle that can access the brain, Dr. Dhar said. She’s been working on nanoparticles for her whole independent career. In a previous pre-clinical study of different forms of polymers, they noticed a small fraction of these nanoparticles may reach the brain. By honing those polymers further, Dr. Dhar’s team developed a nanoparticle that can cross both the blood-brain barrier and the outer membrane of mitochondria.
“There have been a lot of ups and downs to figuring this out, and we’re still working to understand the mechanism by which these particles cross the blood-brain barrier,” Dr. Dhar said.
The team then tested the specialized, drug-loaded nanoparticle in pre-clinical studies and found that they work to shrink both breast tumors and breast cancer cells that were seeded in the brain to form tumors there. The nanoparticle-drug combination also appeared to be non-toxic and significantly extended survival in lab studies.
Next, the team wants to test their method in the lab to replicate human brain metastases more closely, perhaps even using patient-derived cancer cells. They also want to test the drug in preclinical models of glioblastoma, a particularly aggressive brain cancer.
For Dr. Dhar and her team, it’s been rewarding to work on therapeutics at their most basic, chemical and physical levels.
“I’m really interested in polymer chemistry and using that toward medical purposes really fascinates me,” said Akash Ashokan, a University of Miami doctoral student working in Dr. Dhar’s lab and co-first author on the study, along with doctoral student Shrita Sarkar. “It’s great to see that applied toward cancer therapeutics.”
Read the original article on University of Miami.