In the 1920s, when French veterinarian Gaston Ramon realised that adding substances to vaccines could trigger a more potent immune reaction, he threw a bizarre variety of ingredients at the diphtheria vaccines he was studying. His first port of call seems to have been the kitchen cupboard: breadcrumbs, tapioca and oil all made it into his early experiments.
A century on, vaccine boosters – called adjuvants – are far from rudimentary; scientists are now creating them using powerful nanotechnology platforms.
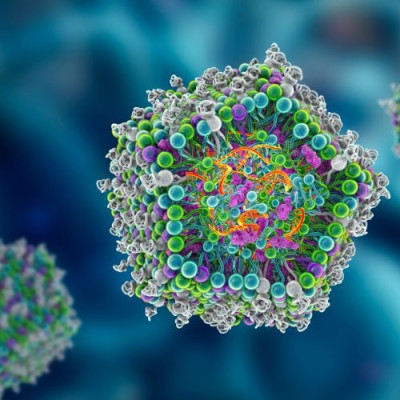
This month, Ben Ou at Stanford University, California, USA and colleagues published a paper in Science describing how they created a nanoparticle platform – resembling a spherical cage – that combines two types of adjuvants.
This new development could mean the production of vaccines that trigger stronger, longer-lasting immunity. The new nanoparticle method could mean that scientists can fine-tune vaccines for different population groups, such as babies or older people, depending on the strength of immune response required.
As the human immune system evolves through our lives, we may be able to use nanotechnology to create vaccines that are especially suited to our own immune systems.
Preparing our defences
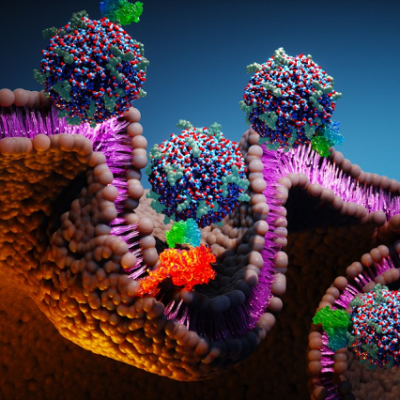
Vaccines ready our immune systems against a potential threat by showing them a hint of a threat. In the main, they show our immune systems an antigen, a part of the pathogen that our bodies are likely to recognise and be able to respond to. In the case of COVID-19, vaccines contained the spike protein that sits on the surface of the SARS-CoV-2 virus as it stimulates a strong immune reaction.
The way the antigen is packaged can vary depending on the vaccine – it might be a killed version of a whole pathogen, a part of one, a protein section, or a piece of RNA or DNA that can code for a pathogenic protein.
When we are given a vaccine, our bodies produce an immediate inflammatory response – immune cells that produce cytokines and other proteins that induce inflammation are triggered. The initial inflammatory response is what can cause the generally harmless, short-term side effects we might feel straight after a vaccine such as a sore arm, redness or a fever.
The antigen is also taken to nearby lymph nodes, which produces a longer-lasting response. Here other types of immune cells such as T cells and B cells produce antibodies and develop a memory for the antigen. These memory immune cells linger, waiting to see if they spot the threat again. Adjuvants try to kick both these immune responses into top gear to ensure immunity that is both strong and long-lasting.
Accidental discovery
The inflammation associated with immunity is what gave Gaston Ramon clues about the use of adjuvants. In his experiments on early diphtheria vaccines, Ramon had noticed that the horses that got infections around the vaccination site had the strongest immune response; his attempts with breadcrumbs and other ingredients were aiming to trigger an infection, and therefore boost the effect of the vaccine.
While Ramon’s experiments were underway in France, across the channel in England, British immunologist Alexander Glenny, also working on diphtheria, found that aluminium salts triggered a strong immune response in rabbits. For decades now, tiny, harmless amounts of aluminium have been the most commonly used adjuvant in vaccines.
Tiny particles, big effects
Adjuvants are increasingly being made using nanoparticles, which allow scientists to have more control over their functionality, helping steer the strength and type of immune reaction they produce.
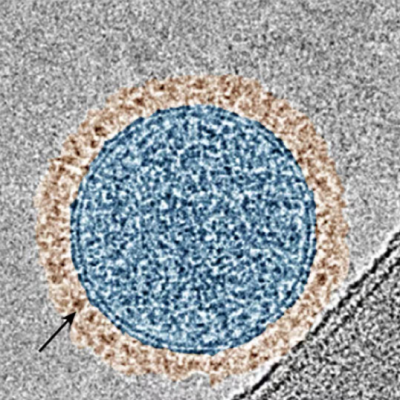
Nanotechnology has been critical in the field of vaccines for a few years now and has been used both for vaccine delivery and as adjuvants. The mRNA COVID-19 vaccines relied on lipid nanoparticles as the delivery vehicles transporting the molecules into our cells. As mRNA is fragile and can be broken down easily, the lipid nanoparticles acted as fatty bubbles protecting the mRNA until it got to where it needed to be.
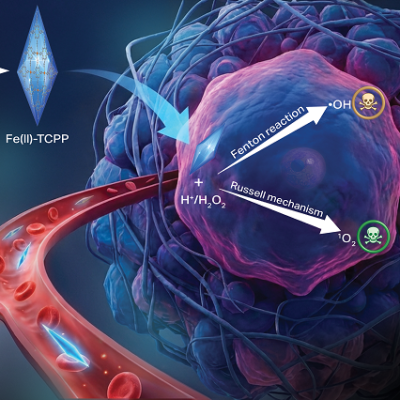
In their recent study, Ben Ou and colleagues built nanoparticle cages made of saponins (immune-stimulating molecules found naturally in plants and animals) and attached toll-like receptor (TLR) agonists. Toll-like receptors are our bodies’ first line of defence as they recognise pathogens and stimulate a variety of immune responses.
When the team tested the new adjuvant platform in COVID-19 and HIV vaccines, the nanoparticle adjuvants triggered a stronger, longer-lasting immune response compared to vaccines containing aluminium.
Different TLR agonists trigger different parts of the immune system, and the researchers experimented with five different combinations of TLR agonists and saponin cages using mice, which elicited different responses.
Although it will be a while before this technology is ready for testing in people, the researchers say that a major win is the fact that this system of dual adjuvants lends itself to customisable vaccines. As the human immune system evolves through our lives, we may be able to use nanotechnology to create vaccines that are especially suited to our own immune systems.
Read the original article on Gavi.