The findings, published May 28 in Proceedings of the National Academy of Sciences (PNAS), could lead to improvements in nanomedicines used for early detection and treatment of kidney damage or disease, as well as disease in other areas of the body.
“Our research findings were surprising and also very significant because they change people’s understanding of how the kidney works at the fundamental level,” said Dr. Jie Zheng, professor of chemistry and biochemistry in the School of Natural Sciences and Mathematics and a corresponding author of the study.
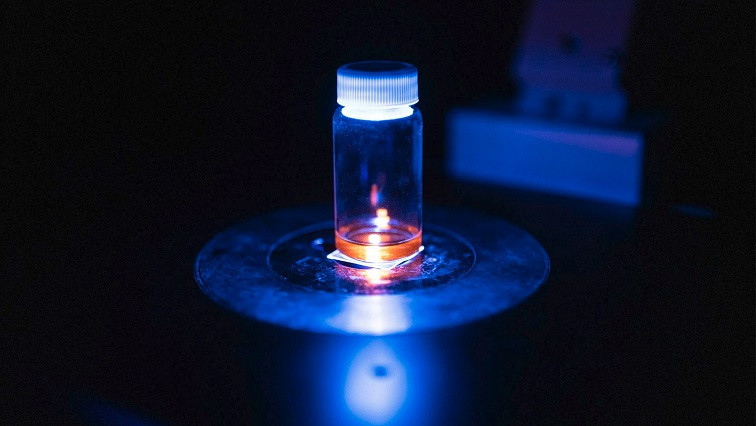
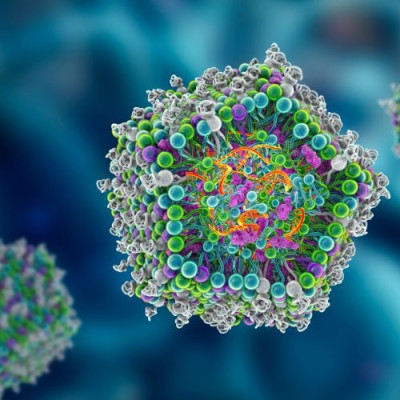
Zheng, who is also a Distinguished Chair in Natural Sciences and Mathematics, and his colleagues coated tiny gold nanoparticles with positively charged chemicals to engineer the surface electric charge of the particles. In mice, they then tracked how the particles traveled through and interacted with various components of the kidney.
“Cell membranes are mainly negatively charged, but the degree of the negative charge may vary depending on the type of cell. Because opposite electric charges attract, putting a positive charge on the nanoparticles significantly enhances their interaction with kidney cells,” said Yingyu Huang PhD’20, a research scientist in Zheng’s lab and the study’s lead author.
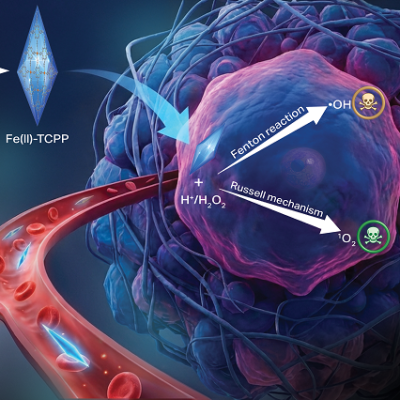
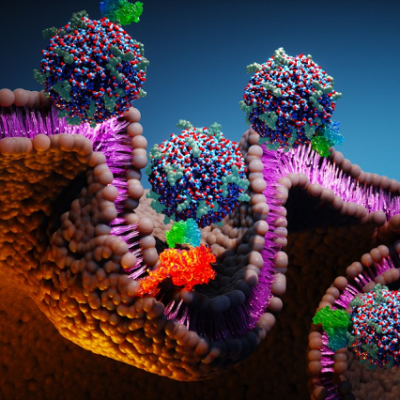
Understanding how the kidney processes substances based on charge is important because nanomedicines, which use nanoparticles to deliver imaging agents and drugs to specific parts of the body, are already in use for diagnosis and treatment of disease and injury, including cancer, Zheng said. Delivery particles eventually must be eliminated from the body, with those smaller than 8 nanometers often leaving through the urinary tract, which starts with the kidneys.
“The kidney is the clearance route to eliminate these particles from the body once they have delivered their payload,” said Dr. Mengxiao Yu, research associate professor of chemistry and biochemistry and a corresponding author of the study. “If we use them to treat other areas of the body, we want to minimize the interaction the particles have with the kidney so that they will pass easily and not damage the organ. On the other hand, treating kidney disease requires stronger nanoparticle interactions with the kidneys. Understanding how charge affects this interaction can help tailor nanoparticles to better meet these needs.”
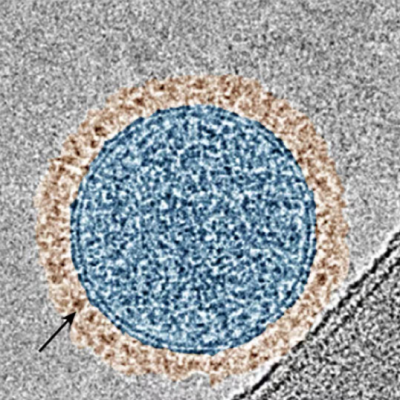
In the kidney, blood flows into millions of filtering units called nephrons, each of which contains a glomerulus — a cluster of tiny blood vessels — as well as tubules and capillaries. Using the nanoparticles as probes allowed the researchers to understand which component of the kidney’s complex structure is most negatively charged.
The results were unexpected.
The researchers found that the proximal tubule was the most negatively charged area and that the peritubular capillary was a secondary barrier to the transport of charged nanoparticles within the kidney. The glomerulus came in third.
“It was previously thought that the glomerulus was the primary charge barrier in the kidney, but our experiments provide clear evidence that that is not true,” Zheng said.
The researchers also determined that when positively charged nanoparticles interact with negatively charged cell membranes, the strength of that attraction is dependent primarily on the distance between the two, in addition to the charge density of each.
According to the Centers for Disease Control and Prevention, chronic kidney disease (CKD), a condition in which a person’s damaged kidneys cannot effectively filter waste from the blood, is a leading cause of death in the U.S. More than 35 million U.S. adults are estimated to have CKD, and most are undiagnosed.
The UT Dallas researchers said a better understanding of how kidney disease or damage changes the electrical charge barriers in kidney cells could inform the design of nanomedicines that target specific diseased sites and leave normal kidney cells unaffected.
“This is important because, for example, in acute kidney injury, the site of major damage is the proximal tubules,” Huang said. “But early damage induced by infectious disease often occurs first in the peritubular capillaries. Our work demonstrates that in the future, we could tune nanoparticles to different kinds of kidney disease.”
The results complement earlier research by the UT Dallas team, which previously determined how the size of nanoparticles is related to their clearance from the kidneys.
“In 2017 we figured out the size barrier. Now we finally figured out the charge barrier, which is much more complicated,” Zheng said.
Read the original article on University of Texas at Dallas.