Middlemen get a bad rap for adding cost and complications to an operation. So, eliminating the go-betweens can reduce expense and simplify a process, increasing efficiency and consumer happiness.
James Dahlman and his research team have been thinking along those same lines for stem cell treatments. They’ve created a technique that eliminates noisome middlemen and could lead to new, less-invasive treatments for blood disorders and genetic diseases. It sidesteps the discomfort and risks of current treatments, making life easier for patients.
“This would be an alternative to invasive hematopoietic stem cell therapies — we could just give you an IV drip,” said Dahlman, McCamish Early Career Professor in the Wallace H. Coulter Department of Biomedical Engineering. “It simplifies the process and reduces the risks to patients. That’s why this work is important.”
Dahlman and a team of investigators from GeorgiaTech, Emory University, and the University of California, Davis, published their approach in the journal Nature Biotechnology.
Minding the Parents
Hematopoietic stem cells (HSCs) are like parent cells. Residing in the bone marrow, they produce all types of cells needed to sustain the blood and immune systems. Their versatility makes HSCs a valuable therapeutic tool in treating genetic blood diseases, such as sickle cell anemia, immune deficiencies, and some cancers.
HSC therapies usually involve extracting cells from the patient’s bone marrow and re-engineering them in a lab. Meanwhile, the patient endures chemotherapy to help prepare their body to receive the modified HSCs.
“These therapies are effective but also hard on the patients,” Dahlman said. “Patients undergo chemotherapy to wipe out their immune systems so the body will accept the therapeutic cells without a fight. The procedure can be life-threatening. We’re hoping to change that.”
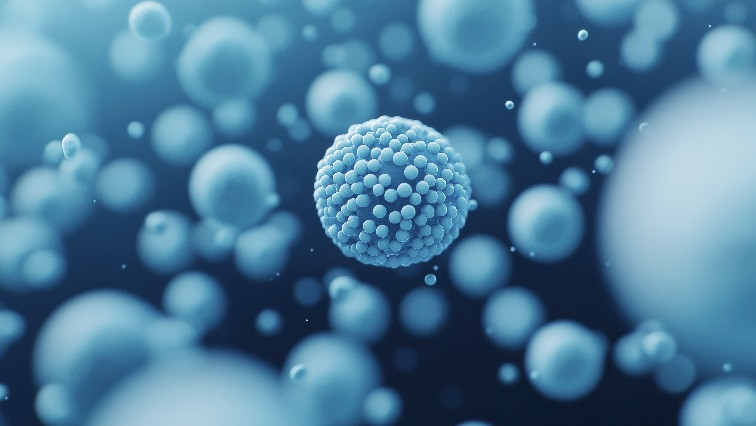
HSCs can also be modified directly inside the body. The procedure uses lipid nanoparticles (LNPs) to carry genetic instructions to the stem cells. The LNPs have targeting ligands attached — molecules designed to find specific target cells. Precisely engineering them adds layers of time, complexity, and cost to the process. They are, like extraction from bone marrow and chemotherapy, another middleman.
The researchers wanted something simpler. They found it in a specific nanoparticle called LNP67.
“Unlike other nanoparticle designs, this one doesn’t require a targeting ligand,” Dahlman said. “It’s chemically simple, which means it’s easier to manufacture and opens the door to eventually scaling production, like mRNA vaccines.”
Overcoming the Liver
The key to LNP67’s success is its ability to dodge the liver, the body’s primary blood filter. Foreign invaders, even helpful invaders delivered through an IV as medicine, can be captured by a healthy liver.
“The liver absorbs almost everything,” Dahlman said. “But, by reducing what it captures by even as little as 10 percent, we can double delivery to other tissues where the nanoparticles and their payloads are needed.”
The researchers developed 128 unique nanoparticles, narrowing the list down to 105 LNPs that didn’t have targeting ligands. These were ultimately screened and evaluated for their performance in delivering genetic instructions (in the form of mRNA) effectively and safely.
LNP67 emerged as the best performer thanks to its stealthy design. For example, the surface is designed to repel proteins and other molecules that would mark the LNP for capture by the liver. This feature helped the particles circulate more evenly in the body and reach the HSCs.
“We achieved low-dose delivery without a target ligand, which is exciting,” Dahlman said. “This is something we’ve been working toward for years, and I’m very happy we got there.”
Read the original article on GeorgiaTech.