In general, diabetic foot ulcers (DFUs) are challenging to manage. Numerous patients with DFUs must undergo amputations each year, which significantly impacts their quality of life. In the United States alone, costs for the treatment of non-diabetic foot ulcers are estimated at $1.38 billion annually. Impaired healing and poor clinical outcomes are associated with DFUs due to underlying problems with blood circulation, nerve damage, immune function, and fibrosis. DFUs that do not heal also have a lower chance of recovery after surgery.
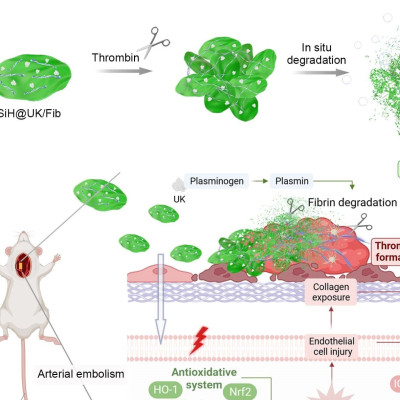
Certain types of cells and molecules must migrate to the wound site during routine wound healing; these cells initiate blood vessel formation and tissue regeneration, which are required for rapid wound repair and closure.
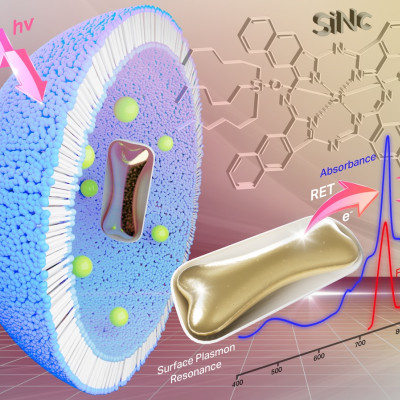
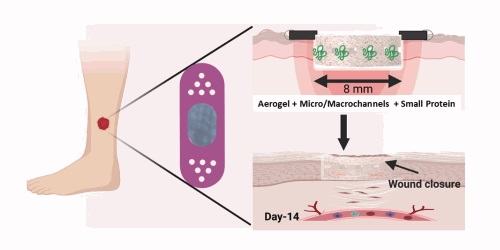
Microarchitecture of dressings is crucial in sustaining the wound structure by allowing cells to migrate through the dressings to close the wound. The UNMC/TIBI team engineered nanofibrous aerogels containing organized microstructure that facilitated cell migration, oxygen, and nutrient delivery to the wound bed.
Moreover, preventing infection is also crucial in the rapid healing of DFUs. The team has incorporated a novel anti-microbial peptide into the dressing to prevent bacterial growth and promote healing. The advantage of this novel peptide is its low-cost and potency compared to commercially available anti-microbial agents.
Using a Type 2 diabetic wound mouse model, the team demonstrated that their novel dressing healed DFUs in 2 weeks which was significantly faster than previous dressings.
“The combined properties of our nanofiber aerogel work synergistically to produce a superior treatment for diabetic wounds,” said Ali Khademhosseini, Ph.D., TIBI’s Director and CEO. “And it offers the potential for use in future biomedical applications.”
Read the original article on Terasaki Institute for Biomedical Innovation.