The study, published in Science Advances, addresses a limitation of chemotherapy. Although chemotherapy is the primary treatment option for most cancers, much of the drug is quickly broken down by enzymes in the body or quickly cleared by the kidneys before it reaches the tumor tissue. Moreover, a large amount of the drug in the system reaches healthy tissues, causing toxic side effects.
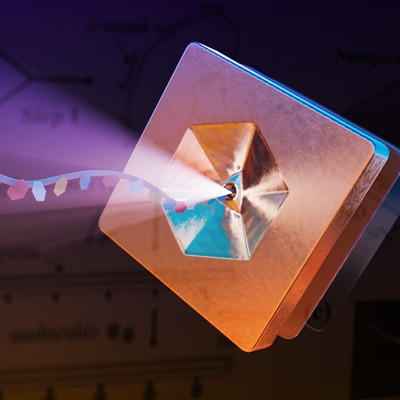
To overcome this challenge, one emerging approach has been to package chemotherapy drugs into nanoparticles. These particles, which are so small they are invisible even under a microscope, can carry chemotherapy agents directly to the tumor. While promising, nanomedicine still needs significant improvement in its ability to deposit the drug into tumor cells.
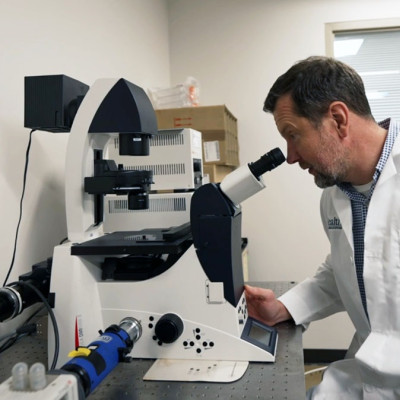
Wenbin Lin, the James Franck Professor of Chemistry at the University of Chicago, is a pioneer in developing nanoparticles for medical imaging and drug delivery. The new study from his lab reports a novel approach to enhance nanomedicine’s effects, which proved effective in mice and which they hope to move to pre-clinical testing.
A better vessel
Chemotherapy drugs reach tumor cells by crossing over from blood vessels into the neighboring tumor tissue. But cancer cells often recruit nearby blood vessels to invade other tissues, and these hastily created vessels are often abnormal—creating irregular blood flow patterns and making it difficult for a drug to penetrate the tumor tissue effectively.
Scientists looked at a particular pathway known as STING, for stimulator of interferon genes. STING activation disrupts the tumor vasculature—the arrangement of blood vessels—and increases the leakiness of blood vessels near the tumor. But previous attempts to activate STING had failed to achieve desired outcomes.
The team found strong antitumor effects with large tumor growth inhibition and high cure rates.
Lin and his team designed a tiny polymer that encapsulates both the STING and the chemotherapy drug. This leverages the unique property of STING activators by delivering them along with chemotherapy drugs, with the idea that STING activation increases the permeability of blood vessels around the tumor and thus will enhance the chemotherapy’s effects.
“We have discovered a novel way to use STING activators to disrupt tumor vasculature to basically enhance drug delivery to tumors without enhancing them to other tissues,” said Lin.
“STING activators haven't worked very well by themselves, but by creating nanomedicine, I think this could also make STING activators work alone or in combination, which I think is an important contribution,” said Ralph Weichselbaum, the Daniel K. Ludwig Distinguished Service Professor, Chair of Radiation and Cellular Oncology at UChicago, and senior author on the new study.
The research team evaluated the antitumor effects of the therapy in multiple kinds of tumors in mice, and found strong antitumor effects with large tumor growth inhibition and high cure rates.
“We noted that radiation activates STING like a pathogen because of the double-stranded breaks introduced by radiation and, importantly, that STING agonists might be useful in cancer therapy,” said Weichselbaum.
The scientists also noted that STING may have other effects beyond the blood vessel permeability. The STING pathway gets activated by invading pathogens like bacteria, viruses, and abnormal DNA of cancer and drives inflammatory response to clear off unwanted cells. STING activation also increases the infiltration of T cells and turns immunologically “cold” tumors to so-called “hot” or inflamed tumors, enabling them to be more responsive to immunotherapy agents like immune checkpoint inhibitors.
This work came out of a long-standing collaboration between the UChicago’s Physical Sciences Division and Biological Sciences Division. “This is one of the highlights of my career to be able to work with Dr. Lin because I have hugely benefitted from his expertise in engineering nanoparticles to solve clinical problems,” said Weichselbaum.
“The next steps are to do more validation studies and prepare for scaling the technology and hopefully testing it in humans,” said Lin.
Read the original article on University of Chicago.